Depression is a serious mood disorder that can cause persistent feelings of sadness and lack of interest, according to the Mayo Clinic. It’s also known as clinical depression or major depressive disorder and can affect how you feel, think, and behave. It can even lead to a range of emotional and physical problems.
“The Mayo Clinic notes that those with depression may experience severe symptoms that impact their daily activities, including work, school, social activities, and relationships. However, the cause of these symptoms may not always be clear.”
According to the U.S. National Institute of Mental Health (NIMH) (citing the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-5]), major depressive disorder involves a minimum period of two weeks during which a person “experiences a depressed mood or loss of interest or pleasure in daily activities and suffers a majority of specified symptoms such as problems with sleep, eating, energy, concentration, or self-worth.”
Here is a list of common symptoms of depression according to the Mayo Clinic:
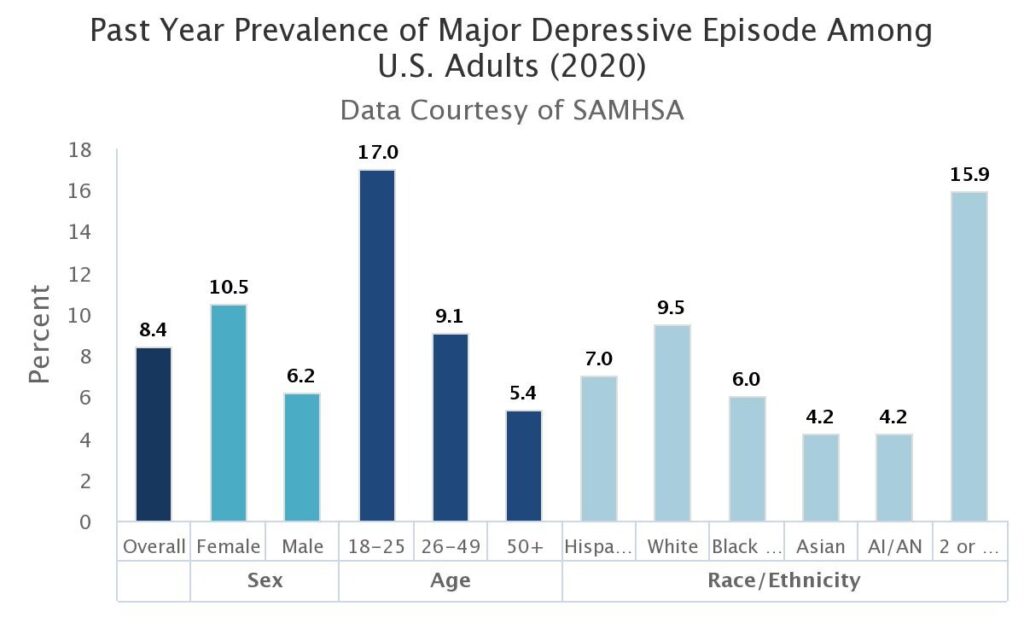
The NIMH states that major depressive disorder is one of the most common mental disorders in the United States, with approximately 21 million adults experiencing at least one major depressive episode in 2020. This equates to over 8% of the adult population.
The organisation also noted that the prevalence of major depressive episodes is higher among adult females (11% of the population) compared to males (6%), and that young people aged 18-25 have the highest rate of depression at 17%.
The U.S. Centers for Disease Control and Prevention (CDC) states that around five percent of individuals aged 18 and above experience “regular feelings of depression.” According to the CDC, almost 11 percent of doctor’s office visits have depression recorded in the medical record. In addition, the CDC reports that over 11 percent of hospital emergency room visits show depression on the official medical record.
Furthermore, depression is the main cause of suicide, with the CDC reporting that 46,000 suicides occur in the United States annually (14 per 100,000 people).
According to the study, depression is described as “a mental health condition that has been shown to be associated with impaired health-related quality of life (HRQoL).” The study notes that it is necessary to address HRQoL in individuals with depression “through a holistic mental health approach, including appropriate pharmacological treatments alongside psychological and social measures.”
The researchers identified several issues with traditional antidepressant medications, including low response rates (about 50 percent, according to one study) and the possibility that their effectiveness may only be for individuals with severe depression rather than those with mild to moderate cases. In addition, the researchers pointed out that there are many potential negative side effects associated with using pharmaceuticals to treat depression.
The study included 129 patients, all of whom had a primary diagnosis of major depressive disorder and an average age of 36. The study participants were mostly male, with 74 percent being male and 26 percent being female. The patients consumed cannabis, which the study referred to as “cannabis-based medicinal products” or CBMPs, in various forms including “sublingual, oral, or vaporised routes of administration.”
The study reported that “vaporised dry flower preparations alone were prescribed to 61 patients (47 percent), oral or sublingual oils alone were prescribed to 21 patients (16 percent), and 33 patients (26 percent) were prescribed both.” A significant percentage of the participants had secondary diagnoses such as anxiety (33 percent) and insomnia (6 percent).
The study discovered that treatment with CBMPs “was associated with statistically significant improvements in depression,” including reduced anxiety and improved sleep. The study participants were surveyed after one, three, and six months of treatment with CBMPs, and improvements in depression, anxiety, and sleep were noted in each survey.

The study authors explained that “theories about the antidepressant effects of CBMPs are centred around the actions of the endocannabinoid system [ECS] and its interaction with other systems.” They pointed out that activation of CB1 receptors in the prefrontal cortex and hippocampus regions of the brain—which are an important part of the ECS—have “been linked to antidepressant effects.”
During the six-month period of CBMP consumption, some adverse events were reported. In total, 14 percent of the study subjects experienced adverse events, with the most common being fatigue and insomnia.
The research report concluded that “treatment with CBMPs was associated with improvements in depression after one, three, and six months of treatment” in patients with major depressive disorder in the United Kingdom. It found that cannabis use among individuals with severe depression was associated with “improvements in anxiety, sleep quality, and overall HRQoL.”
The researchers summarised their findings by stating: “This suggests that CBMPs could have antidepressant effects, although the limitations of the study design mean that a causal relationship cannot be proven.”
source: https://www.tandfonline.com/doi/full/10.1080/14737175.2022.2161894